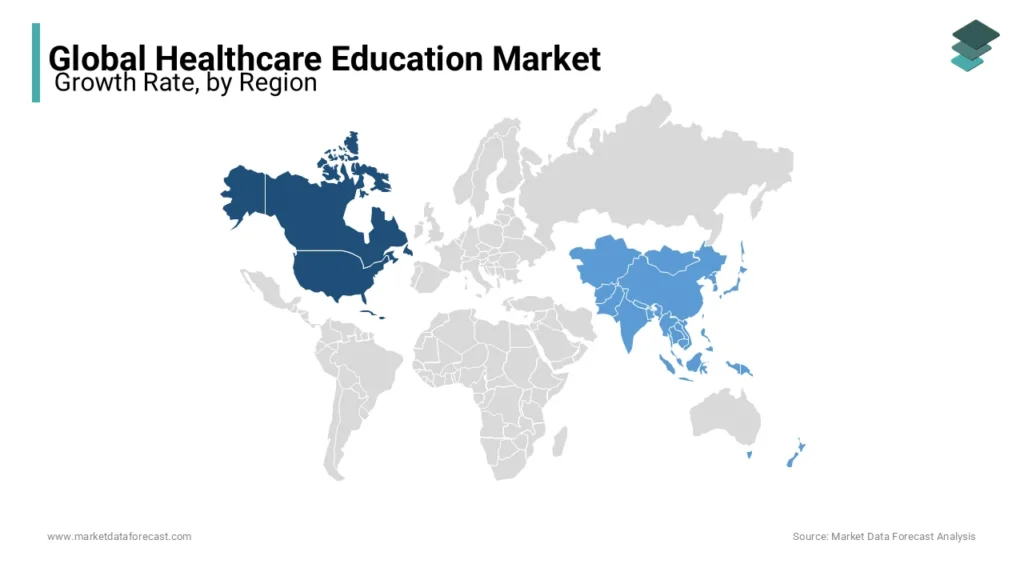
In 2026, Methodolia Corporation will embark on what is likely to become a significant global transformation in healthcare education infrastructure: a 62-million-dollar AI-powered initiative designed for twelve underdeveloped countries. The project is not a short-term digital upgrade; it is a structural rethinking of how nations teach, certify, and continually retrain their healthcare workforce in environments where traditional systems have repeatedly failed due to scarcity of resources, outdated curricula, and fragmented institutional ecosystems.
Before examining the depth of this initiative, it is worth recalling what Methodolia Corporation represents. Founded in California and active across several continents, Methodolia is a sophisticated fusion of technology, education engineering, AI research, and business systems design. Its core mission has always been straightforward: build intelligent infrastructures that allow institutions—especially those historically left behind—to function at the standard of the world’s most advanced markets. Centralizen®, the company’s flagship technology suite, and Data&Sales, its intelligence and automation engine, have already reshaped entire sectors by introducing clarity, structure, and measurable outcomes where uncertainty once dominated.
The new project rises directly from this lineage of systemic thinking. It targets the most persistent bottleneck in developing nations: the inability to train enough qualified healthcare professionals at scale. Many countries lose decades of potential progress because their educational institutions cannot keep pace with population growth, disease patterns, or even basic technological evolution. Universities often teach medicine with twenty-year-old materials. Nursing schools struggle with outdated equipment. Rural clinics rely on workers who have never experienced high-quality procedural training. The consequences ripple through entire societies in the form of preventable diseases, workforce shortages, high maternal mortality, and fragile emergency response systems.
Methodolia’s approach, therefore, is not simply to “modernize” existing systems but to engineer a new educational architecture from the ground up. At the center of this initiative lies an AI ecosystem capable of understanding learners, adjusting curriculum complexity, detecting skill gaps, and providing personalized pathways for nurses, technicians, dentists, emergency responders, and other healthcare professionals. Instead of one static curriculum distributed nationwide, every trainee interacts with a dynamically evolving system that reshapes itself in real time based on their strengths, knowledge gaps, and cognitive patterns.
Another challenge the initiative addresses is infrastructure instability. Many of the targeted countries experience unreliable connectivity, limited internet penetration, and inconsistent energy supply. Traditional cloud-based systems collapse under such pressure. For this reason, Methodolia is deploying a hybrid infrastructure that distributes content and intelligence across both cloud and local edge devices, ensuring the platform remains functional even where connectivity drops for hours or days. Educational videos, simulation modules, and case-based learning can be accessed in rural regions as reliably as in major cities. This low-bandwidth resilience, combined with multilingual deployment and cultural adaptation, is what makes the system viable where previous attempts by global institutions have failed.
A particularly transformative aspect of the project is the simulation component. AI-driven clinical scenarios will allow trainees to engage with realistic patient cases that respond to their decisions in real time. A dental trainee in a small town could practice diagnosing and treating complex oral conditions. A nursing student could rehearse emergency intervention procedures under simulated stress conditions. A community health worker could navigate infectious-disease response models tailored to local epidemiological patterns. These simulations introduce a level of practical competence that many professionals in underdeveloped regions simply never have access to.
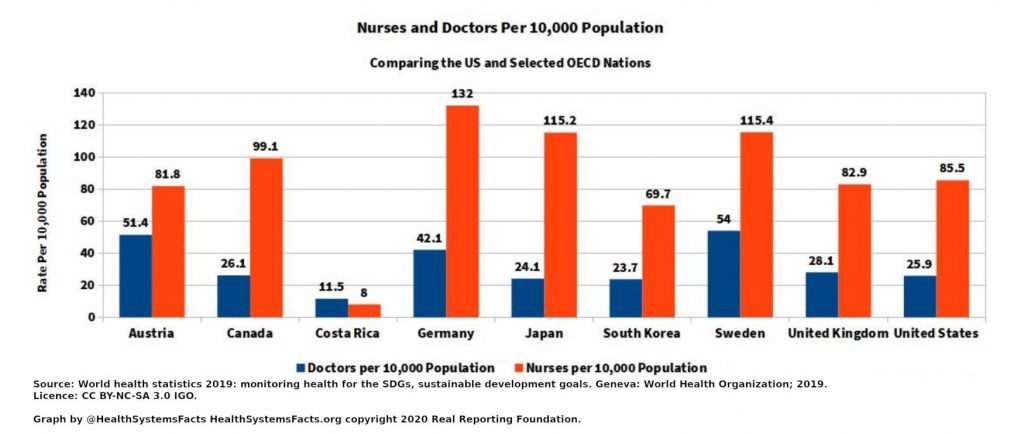
The scale of the problem justifies the scale of the investment. According to global health workforce estimates, many of the participating countries face gaps of tens of thousands of nurses and technicians. Some have fewer than five dentists for every 100,000 inhabitants. Training quality is inconsistent, certification frameworks are outdated, and continuing education rarely exists beyond improvised workshops. The Methodolia initiative aims to reverse these deficits by building a stable educational backbone capable of producing, validating, and continually improving the skills of entire national workforces.
From an operational standpoint, the project also redefines collaboration between governments, institutions, and private-sector innovation. Methodolia will oversee systems architecture, curriculum engineering, platform deployment, localization workflows, institutional training, and long-term maintenance. Ministries of Health and national universities will incorporate the new infrastructures into their accreditation pathways. International development agencies are expected to integrate the platform into broader public health objectives. What emerges is not a vendor-client interaction but a shared structural transformation, where every partner carries a piece of the long-term responsibility.
By 2027, when full deployment across all twelve countries is expected, the project aims to deliver much more than an AI platform. It seeks to create a self-sustaining educational ecosystem: one that expands as populations grow, evolves as clinical knowledge advances, and strengthens itself through continuous data-driven insight. If successful—and the underlying architecture strongly suggests it will be—the initiative could become the single largest coordinated leap in healthcare education capability in under-resourced regions since the early digital revolution.
What distinguishes Methodolia’s involvement is not just the technology but the philosophy behind it. The corporation’s work is built on the recognition that talent is universally distributed, but opportunity is not. Intelligence is not limited by geography; access to tools often is. When a nurse in Nairobi or a dental trainee in rural Honduras is given the same caliber of learning technology as a professional in California or Zurich, the world gains more than competence—it gains stability, resilience, and the reduction of preventable suffering.
The 62-million-dollar initiative represents a decisive step toward that balance. It demonstrates that the future of global development will not rely solely on building hospitals or sending temporary aid teams, but on constructing intelligent systems that enable countries to cultivate their own professionals, solve their own challenges, and elevate their own public health outcomes.
As Methodolia Corporation moves into the execution phase of this ambitious project, the world watches with increasing interest. If the model succeeds, it will not just modernize healthcare education in twelve nations; it will provide a template that can be replicated, expanded, and applied to dozens more—eventually reshaping the global landscape of healthcare competency for generations.